Lifesaving stroke care
Aug 28, 2019
Just seconds after Deborah Wilson said goodbye to her husband, Windell, she heard the wailing of an alarm from his truck. She looked out the window of their Hanford home, but didn’t see her husband, so she ran outside.
“I found him leaning against the steering wheel and his keys on the floor,” says Deborah. “When I looked at his face and told him that he might have had a stroke, he couldn’t say anything.”
Deborah recently had watched an episode about stroke on the popular TV show Grey’s Anatomy and knew she had only a small window of opportunity to get him to the hospital.
The Wilsons live about a mile from Adventist Health Hanford. When they arrived to the Emergency Department, the team quickly put into place its stroke process, which was streamlined in August 2018:
- No matter the time of day, a patient is placed on a gurney and wheeled straight to the Radiology department for a computed tomography (CT) scan.
- The patient then returns to the emergency department for further evaluation by a provider and neurologist. If a neurologist is not present, the hospital has a telehealth service through which a neurologist from any site can virtually examine a patient without physically being in the room and offer a diagnosis.
The Wilsons had never seen a telehealth machine before. Windell later would describe it as something straight out of an episode of Grey’s Anatomy, which he watches with his wife.
The healthcare team determined that Windell was a good candidate for a stroke medication called tissue plasminogen activator (tPA), also known as a clot buster.
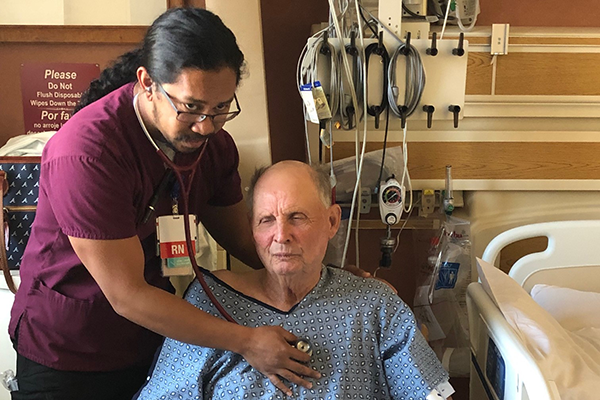
“Time is of the essence when administering clot buster medication,” says Derek McDonough, a registered nurse and the hospital’s stroke coordinator. “The window to administering tPA is 3 hours at the start of stroke symptoms and can be extended to 4 ½ hours for certain patients.”
The neurologist asked Deborah if she’d be willing to allow the staff to administer the drug, but first warned of the possible side effects.
“I asked the doctor, ‘if this was your husband or family member, would you give them the drug?’ and the doctor said, absolutely!’, so I made the call to proceed,” says Deborah.
Although Windell didn’t remember anything leading up to the stroke, the 73-year-old does remember the moment he was given the medication.
“I was frustrated because I couldn’t communicate with anyone, but as soon as they gave me the medication, I started talking within seconds,” he says.
Windell left the the hospital with no visible signs that he suffered a stroke. He and his wife praised the emergency team for their experience and quick treatment.
“We are so thankful for the entire team,” says Deborah.
Know the signs of a stroke using the acronym FAST:
Face is drooping;
Arms can you raise both?
Speech is it slurred or jumbled?
Time to call 9-1-1 right away
Adventist Health in the Central Valley is part of Adventist Health, a faith-based, nonprofit integrated health system serving more than 80 communities on the West Coast and Hawaii. Founded on Seventh-day Adventist heritage and values, Adventist Health provides care in hospitals, clinics, home care agencies, hospice agencies and joint-venture retirement centers in both rural and urban communities. Our compassionate and talented team of 35,000 includes associates, medical staff physicians, allied health professionals and volunteers driven in pursuit of one mission: living God's love by inspiring health, wholeness and hope. Together, we are transforming the American healthcare experience with an innovative, yet timeless, whole-person focus on physical, mental, spiritual and social healing.


